|
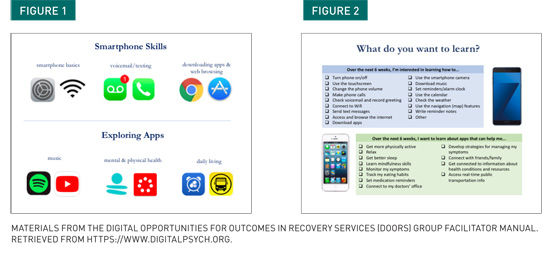
The rise of digital health technology presents novel opportunities for enhancing clinical services and supporting individuals living with mental illness in their recovery. As the cost of smartphones has decreased over time, access to this technology has steadily risen, paving the way for wider engagement with digital health tools and resources (Firth et al., 2016). Research related to digital health has grown exponentially in the past five to 10 years as thousands of smartphone apps targeting a plethora of health conditions have flooded the marketplace (Chandrashekar, 2018). For many vulnerable populations, however, this technology still remains inaccessible (Büchi, Festic, & Latzer, 2018). Individuals experiencing mental illness may own smartphones but may not have the technical skills to participate in the digital world and to utilize health-related technology to its fullest potential. Because it is the exception, not the rule, for individuals with lived experience to play a central role in the development of mental health–related apps, many of the barriers related to users’ digital skills and knowledge have been overlooked. In digital health research and development, the prevailing notion of “if you build it, they will come” discounts the experience of individuals with limited tech competencies and limited access to digital learning opportunities. As a result, people with serious mental illness (SMI) often cannot access the very tools that are being developed for their benefit. Without digital skills, vulnerable populations cannot access the wealth of resources available to those with more advanced technical competencies. The divide between those who have the skills to engage with digital opportunities and those who do not presents an opportunity for social workers to advocate for digital equity and inclusion. Access should not be a privilege but rather a right for all who wish to participate in the digital world. In pursuing social change on behalf of vulnerable populations, social workers can help bridge this divide by promoting digital skill development and incorporating smartphone tools into clinical care. Digital Health Literacy Skills Training Our aim is to help individuals with lived experience to engage safely and meaningfully with the digital health world. Group participants are viewed as the experts on their own experience, and the curriculum can be adapted to meet the learning needs of each individual. We have implemented DOORS within a first episode psychosis day program as well as in two drop-in centers for individuals with chronic schizophrenia, each time altering the group content to better meet participants’ needs. The content areas include digital skill building, setting technology supported wellness goals, capturing lived experience, and evaluating apps. Our group facilitator manual provides guidance for clinicians interested in running digital health groups and is available through our team website (www.digitalpsych.org). Digital Skill Building
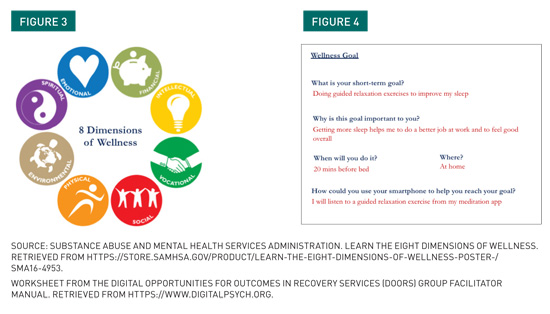
Technology-Supported Wellness As a group, clients explored the step count feature within the Apple Health and Google Fit apps and helped participants set small actionable exercise goals that they could measure with the help of their smartphone. Participants enjoyed sharing their weekly step count data with the group and provided encouragement to one another in reaching their exercise goals. Gaining awareness of their physical activity prompted discussions on strategies for weaving exercise into daily life and exploration of other digital tools related to physical health. While digital mental health research often focuses on symptom tracking and disease management, we realized that some of the more practical smartphone features support additional areas of wellness (e.g., social, vocational, intellectual) that can influence participants’ mental health. Many participants struggled with using their smartphones to communicate with their friends, families, and health care providers and wanted to learn how to check voicemail and send text messages. For others who needed support in staying organized, we explored the smartphone notepad and calendar app features. Transportation apps were also of particular interest to participants who rely on public transportation to get to doctor’s appointments, day programs, and their places of employment. While these digital tools are not considered “health” apps, they may still play a role in supporting people with SMI to make progress in their recovery.
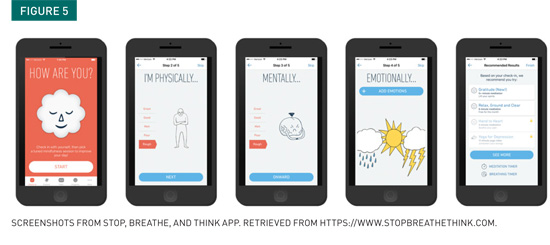
Capturing Lived Experience
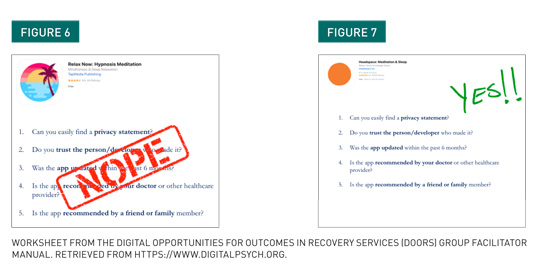
Informed Decision-Making
DOORS Learnings Advancing Social Change — Liza Hoffman, MSW, LICSW, is clinical director of the digital psychiatry division at Beth Israel Deaconess Medical Center.
References Chandrashekar, P. (2018). Do mental health mobile apps work: Evidence and recommendations for designing high-efficacy mental health mobile apps. mHealth, 4, 6. Firth, J., Cotter, J., Torous, J., Bucci, S., Firth, J. A., & Yung, A. R. (2016). Mobile phone ownership and endorsement of “mHealth” among people with psychosis: A meta-analysis of cross-sectional studies. Schizophrenia Bulletin, 42(2), 448-455. Henson, P., David, G., Albright, K., & Torous, J. (2019). Deriving a practical framework for the evaluation of health apps. The Lancet Digital Health, 1(2), e52-e54. |

 Social Services Innovations — Equity and Inclusion in Digital Mental Health Literacy
Social Services Innovations — Equity and Inclusion in Digital Mental Health Literacy