|
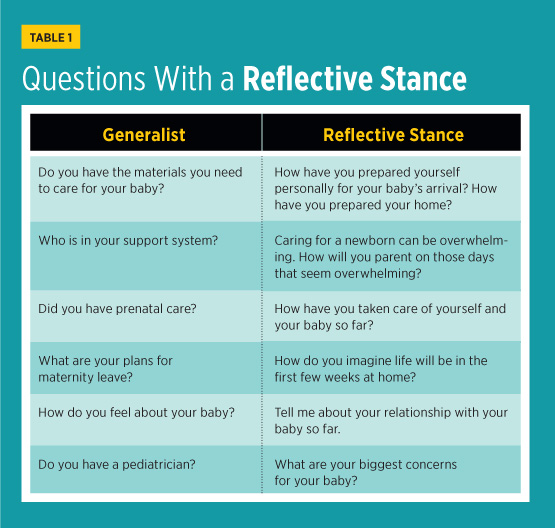
By taking a reflective stance, providers and social workers can bolster the health of children and families. Early caregiving relationships have a profound effect on infant neurological, cognitive, social, and emotional development across the lifespan. Therefore, the American Academy of Pediatrics has recommended attending to infants’ social-emotional development and their relationships with primary caregivers.1 By assessing and working with families alongside pediatricians in acute care, hospital social workers (HSWs) are well positioned to implement this recommendation. Adopting a “reflective stance” in assessment, intervention, and documentation in the medical record can expand opportunities to understand parents’ thoughts and emotions around infant care and initiate dialogue about social-emotional development between families and providers.2 Attachment and Being Reflective Caregivers who consistently attend to the infant’s attachment cues and respond in ways that support the infant’s developing sense of self and need for safety and autonomy provide a secure base and foster secure attachment.3,5 Sensitive caregiving, or the ability to accurately interpret the infant’s signals and respond appropriately, is the cornerstone of secure attachment. It is supported by the parents’ ability to reflect on the infant’s internal states and to see the infant as a unique person with their own experiences of the environment and of relationships. Parents’ capacity to understand their own and their infant’s behavior in terms of underlying mental states (eg, desires, motivation) and to acknowledge that, at times, mental states are difficult to discern is called parental reflective functioning (RF).6,7 Parental RF is associated with maternal sensitivity and infant/toddler attachment security.8,9 Research has shown that parents vary in their capacity for RF, and limited RF relates to less sensitive caregiving and to insecure attachment. A parent with limited RF may misinterpret the infant’s behavior and make distorted or malevolent attributions that undermine the attachment relationship and the infant’s developing sense of self.10 For example, a mother with limited RF may perceive her infant’s night waking as a manipulation or an intention to keep her awake when she is tired. Consequently, the mother might respond to the infant insensitively instead of trying to understand the infant’s needs. An HSW could hear evidence of limited RF when a mother states that her newborn is difficult “on purpose” or that the infant “knows just when to cry” to keep her awake. These statements indicate potential RF problems and should be a cue for the HSW to further assess the mother’s thinking around her relationship with her infant. Taking a Reflective Stance Ordway and colleagues advocate for pediatric health care providers to use RF in practice with families by taking a “reflective stance” in interactions.2,11 When taking a reflective stance, a provider uses reflective language, open-ended questions, and genuine curiosity to prompt parents to think about their children’s experiences. In a parallel process, the provider models RF to the parent. The provider might ask a father what he thinks the infant feels during an exam, or comment on the infant’s nonverbal cues during a well-child check. These questions invite a deeper discussion about social and emotional health and family relationships. Also, they signify to the parent that the provider understands the child as a psychological being with thoughts and feelings, providing a model for the parent to do the same. A reflective stance could work similarly for HSWs as they gather information to conceptualize problems and strengths and decide whether there is a need for parenting supports or cause for concern about maltreatment. Asking questions that cue parents to share their thoughts and feelings about the infant and their parenting could help HSWs clarify presenting problems and make more informed assessments and treatment plans. For example, instead of asking whether a family has a car seat to take the infant home, the HSW might ask the family how they have prepared for the birth. This shift in questioning invites a richer discussion about the family’s thinking around the birth, allowing the HSW to gain insight into the family’s readiness and capacity to care for the child. Reflection in Assessment To address this gap, HSWs can use a reflective stance to gain important information about infant mental health and parenting. Measuring Parental RF Instead of, or in addition to, relying on measures to learn about RF, HSWs could use the engagement skills that they already know (eg, open-ended questions, paraphrasing) with a reflective stance in mind. For example, suppose that the HSW receives a referral to see an adolescent mother who gave birth to her third child. Having had her parental rights revoked for her first two children, the mother worries about whether she will be able to parent this child. The medical staff shares those concerns. In this instance, there is much to gain by asking the mother questions from a reflective perspective. Table 1 offers examples of assessment questions with a more reflective lens that may be useful in this case.
While the differences between the questions in Table 1 may be subtle, the shift to reflective questions centers the conversation on the infant’s social-emotional health and the parent-child relationship. They also provide insight into the parent’s state of mind with respect to parenting. For instance, if questioned about maternity leave, the mother might state that she is not employed and has no need for maternity leave. Instead, asking about the mother’s expectations for the first few weeks at home gives her opportunities to share about whether she has given thought to how to care properly for a newborn. At times, direct questions such as, “Have you used substances during pregnancy?” are necessary. Nevertheless, a reflective follow-up adds a deeper knowledge of parenting capacity. Furthermore, questions from a reflective stance invite parents to think in new ways about the child, generating more insightful discussion and foregrounding parents’ self-identified strengths. Reflection in Interactions The parent’s response provides insight into their understanding of Jesse and helps the HSW create an effective treatment plan. If the mother says, “Jesse chooses when he wants to eat,” or “He is picky about food,” further exploration of RF, developmental expectations, and sensitive caregiving may be warranted. These comments indicate that the mother misunderstands Jesse’s behavior and developmental capacities. Also, she may be unable to accurately perceive her child’s internal states. Conversely, if she attempts to understand Jesse’s experience or talks about the strategies that she has used to help him succeed with feedings, she may need additional education or medical guidance rather than intervention. In both cases, the treatment plan follows the reflection-oriented case conceptualization. Asking reflective questions and making reflective statements are useful tools to understand the parent-child relationship. Additionally, HSWs can take the infant’s perspective to focus attention on the child’s internal states. For example, the HSW may narrate from the infant’s perspective: “I am crying and I am not sure why. Maybe my stomach is upset or maybe I need to be held.” These statements, which suggest that Jesse has internal experiences, can generate curiosity about how to care for him in a way that satisfies his needs and provides comfort. By incorporating this approach, the HSW models reflection in a parallel process for the parent. Likewise, the HSW could use reflection to support the mother’s experience with a question such as, “You have two older children at home; what is it like for you to feed Jesse while you also spend time with them?” This demonstrates the HSW’s interest in understanding the mother’s point of view, while engaging her in a discussion about how to address the relationship-based and emotional aspects of Jesse’s diagnosis. Reflection in Documentation
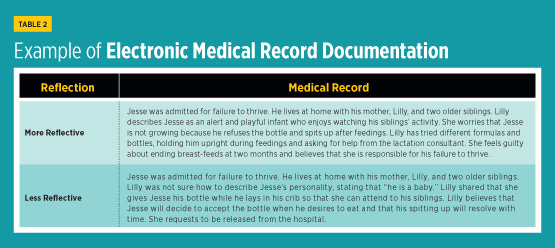
Table 2 provides an example of how to infuse reflection in the EMR. These examples include mental state language (eg, desire, think, worry) that signifies the reflective stance and helps convey the mother’s thinking around her role in Jesse’s health. In the first example, her description of Jesse as alert and playful and of strategies to help him feed shed light on how she thinks about him and their relationship. She is likely more reflective, attempting to figure out how Jesse feels and talking about guilt and hope for improvement. The second example provides a different frame for understanding Jesse’s case. Jesse’s mother seems less reflective as she struggles to talk about his personality and her limited attempts to help him resolve feeding problems. By documenting with a reflective stance, the HSW articulates the presenting problem for the medical team in a way that drives a treatment plan attuned to the family’s dynamics. Conclusion — Ann M. Matthews, PhD, LCSW, is an assistant professor of social work at Nebraska Wesleyan University and a social worker at Bryan Medical Center. Matthews studies infant and maternal well-being and methods for assessing social-emotional health in families in acute and ambulatory care. — Julia Torquati, PhD, is a professor in the department of child, youth, and family studies at the University of Nebraska-Lincoln and the Buffett Early Childhood Institute Community Chair in Infant Mental Health. Her scholarship focuses on the role of relationships in early child development, particularly attachment and self-regulation. — Danielle Swanson, LCSW, has been a social worker in Lincoln, Nebraska, for over a decade, spending most of her career at Bryan Medical Center before moving to school social work at Lincoln Public Schools. She has expertise in assessing and working with new parents and families with children.
References 2. Ordway MR, Webb D, Sadler LS, Slade A. Parental reflective functioning: an approach to enhancing parent-child relationships in pediatric primary care. J Pediatr Health Care. 2015;29(4):325-334. 3. Ainsworth MD. Patterns of infant-mother attachments: antecedents and effects on development. Bull N Y Acad Med. 1985;61(9):771-791. 4. Sroufe LA, Egeland B, Carlson EA, Collins WA. The Development of the Person: The Minnesota Study of Risk and Adaptation From Birth to Adulthood. New York, NY: Guilford Press; 2005. 5. Main M. The organized categories of infant, child, and adult attachment: flexible vs. inflexible attention under attachment-related stress. J Am Psychoanal Assoc. 2000;48(4):1055-1096. 6. Luyten P, Mayes LC, Nijssens L, Fonagy P. The parental reflective functioning questionnaire: development and preliminary validation. PLoS One. 2017;12(5):e0176218. 7. Slade A. Parental reflective functioning: an introduction. Attach Hum Dev. 2005;7(3):269-281. 8. Ensink K, Borelli JL, Roy J, Normandin L, Slade A, Fonagy P. Costs of not getting to know you: lower levels of parental reflective functioning confer risk for maternal insensitivity and insecure infant attachment. Infancy. 2019;24(2):210-227. 9. Krink S, Muehlhan C, Luyten P, Romer G, Ramsauer B. Parental reflective functioning affects sensitivity to distress in mothers with postpartum depression. J Child Fam Stud. 2018;27(5):1671-1681. 10. Schechter DS. On traumatically skewed intersubjectivity. Psychoanal Inq. 2017;37(4):251-264. 11. Ordway MR, Sadler LS, Dixon J, Slade A. Parental reflective functioning: analysis and promotion of the concept for paediatric nursing. J Clin Nurs. 2014;23(23-24):3490-3500. 12. National Association of Social Workers. NASW standards for social work practice in health care settings. https://www.socialworkers.org/LinkClick.aspx?fileticket=fFnsRHX-4HE%3D&portalid=0. Published 2016. 13. Browne T, Keefe RH, Ruth BJ, et al. Advancing social work education for health impact. Am J Public Health. 2017;107(S3):S229-S235. 14. Connolly S. Everyone's business: developing an integrated model of care to respond to child abuse in a pediatric hospital setting. Soc Work Health Care. 2012;51(1):36-52. 15. Svärd V. Assessing children at risk: organizational and professional conditions within children's hospitals. Child Fam Soc Work. 2017;22(S4):81-91. 16. Pajulo M, Tolvanen M, Pyykkönen N, Karlsson L, Mayes L, Karlsson H. Exploring parental mentalization in postnatal phase with a self-report questionnaire (PRFQ): factor structure, gender differences and association with sociodemographic factors. The Finn brain birth cohort study. Psychiatry Res. 2018;262:431-439. 17. Council on Community Pediatrics, Gorski PA, Kuo AA. Community pediatrics: navigating the intersection of medicine, public health, and social determinants of children’s health. Pediatrics. 2013;131(3):623-628. 18. Dworkin PH, Garg A. Considering approaches to screening for social determinants of health. Pediatrics. 2019;144(4):e20192395. |

 Infant Mental Health in Hospital Social Work Practice
Infant Mental Health in Hospital Social Work Practice